Introducing Non-Violent Resistance (NVR)
In March 2022, Rachel Horn and I began training in Non-Violent Resistance (NVR).
NVR has been shown to reduce aggression and improve dynamics within residential and inpatient settings (van Gink et al., 2020; Embeita & Birch, 2025).
Inspired by its use within our then consultant, Dr Claire Purcell’s previous context, we sought to integrate NVR into the ward, family therapy and parent group interventions.
 Integrating Non-Violent Resistance (NVR) in Inpatient CAMHS
Integrating Non-Violent Resistance (NVR) in Inpatient CAMHS
Securing support for NVR training required persistence, but with funding from Health Education England and local underspend, we launched a pilot project across three wards. In collaboration with NVR trainers Lydia Stafford and Nicky Maund, staff received training supported by nursing managers and the matron. The outcomes were striking: morale improved, a shared language of practice developed, and staff reported greater safety, resilience, and agency—benefiting both teams and young people.
A year later, feedback highlighted NVR’s transformative impact. Staff described applying its principles professionally and personally, noting improved patient experiences, reduced incidents and restraints, and enhanced team connection. Sustainability has been achieved through ongoing supervision, integration into daily routines, and inclusion in induction for new staff. This fits with the NHS England Culture of Care Standards (2024), which emphasise relational safety and trauma-informed practice.
Challenges and Collective Responses
Inpatient CAMHS work is complex and emotionally demanding. Staff face trauma exposure, systemic pressures, and experiences of racism and violence (Hunt, 2020; McNicholas & O’Connor, 2023). We addressed these challenges collectively through “announcement letters” affirming shared stances against racism and violence, and reflective rituals such as the “rainbow basket,” celebrating humour, resilience, and solidarity. These practices strengthened team cohesion and well-being, essential for sustaining therapeutic care.
Presence, Erasure, and Mattering
Presence
Omer (2003 in 2022) describes presence as the readiness of adults to act with relational boundaries that young people experience as meaningful. In inpatient CAMHS, cultivating presence is challenging amid distress and systemic fragmentation. Simple, consistent gestures—sitting with a young person at meals, initiating conversation, or “showing up” during tension—create predictability and safety. Reflective supervision helps staff recognise and sustain presence, framing relational steadiness as therapeutic success even without immediate behavioural change.
Erasure
When presence falters, the risk of erasure emerges—moments when clinicians feel their relevance has diminished (Beckers, Jakob & Schreiter, 2021). Erasure can result from rejection by young people, systemic constraints, or lack of organisational support. Structured team reflections, such as baskets and announcement letters, counter this by giving staff voice and visibility. Debriefs following incidents further validate effort and persistence, reinforcing that presence itself has value. Peer recognition becomes a quiet form of resistance against erasure.
Mattering
Mattering—the belief that one’s actions hold significance—sustains professional identity and resilience (Beckers et al., 2022; Jakob, 2025). It reframes experience from “I could do nothing” to “I did what I could,” positioning care as persistence rather than perfection. Recognition through team days, appreciation practices, NVR newsletters, and opportunities to share learning fosters agency and pride. The team’s Trust Star Award for innovation symbolised this collective achievement.
Shared narratives strengthen mattering by validating that therapeutic impact often lies in continuity rather than outcomes. Remaining present with young people, even amidst rejection or uncertainty, embodies the essence of NVR: that steadfast, compassionate presence is both resistance and care.
Conclusion
This journey has not been linear, and it has not been easy. There have been storms: systemic pressures, incidents of violence, racism, and times when staff and young people alike have felt invisible or powerless. And yet, there has also been sunlight: small relational gestures, renewed hope through training, moments of laughter, and the deep pride of watching teams persist and grow.
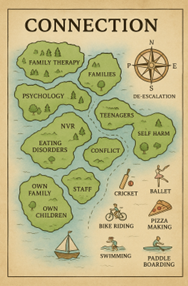
Non-Violent Resistance has given me a framework — but more than that, it has been a compass and a map. It has helped me to resist the sense of erasure when efforts feel unseen or rejected. And it has reminded me, again and again, that we matter — as staff, as teams, and as people who choose to keep showing up.
I hold onto the belief that our presence itself is an act of resistance and care. By continuing to show up for young people, for families, and for one another, we create the possibility of safety, connection, and change, even in the most challenging environments. That, for me, is the anchor, the map, and the compass that keeps me steady in this work.
Written by Collette Williams,
Systemic Family Therapist
Sapphire Lodge, Becton Inpatient CAMHS, Sheffield
NVR Association (NVRA) Accredited Practitioner
Accreditation Module Participant, 2025
References
Beckers, W., Jakob, P., & Schreiter, M. L. (2021). Mattering and parental presence in systemic therapy using nonviolent resistance: The utilization of imaginary methods. Family Process, 61(2), 507–519.
Beckers, W., Jakob, P., & colleagues. (2022). [Further work on mattering and presence].
Burnham, J. (2018). Developments in Social GRRRAAACCEEESSS: visible–invisible and voiced–unvoiced. In Culture and Reflexivity in Systemic Psychotherapy (pp. 139–160). Routledge.
Dulberger, D. (2023). Presentation: The presence mind. EFJCA Congress 2023. Retrieved from https://www.efjca.eu/doc/congres-2023/presentaties/Presentation-Dan-Dulberger.pdf
Embeita, C., & Birch, S. (2025). Non-violent resistance as an intervention for parents of children who present with violent and controlling behaviour: A review of empirical evidence. Educational Psychology in Practice, 41(3), 353–373.
Hunt, L. (2020). Exploring staff wellbeing and trauma exposure in CAMHS inpatient settings (Doctoral thesis, University of Essex).
Jakob, P. (2018). Non Violent Resistance Advanced Level Manual NVR Certificate Course: Working with Trauma. Partnership Projects UK.
Jakob, P. (2025). Nonviolent Resistance in Trauma-Focused Practice: A Systemic Approach to Therapy and Social Care. Routledge.
McNicholas, F., & O’Connor, C. (2023). Measuring experience of inpatient child and adolescent mental health services. International Journal of Environmental Research and Public Health, 20(11), 5940.
NHS England. (2024). Culture of Care Standards for Mental Health Inpatient Services. Retrieved from https://www.england.nhs.uk/long-read/culture-of-care-standards-for-mental-health-inpatient-services/
Omer, H. (2022). Non-Violent Resistance: A New Approach to Violent and Self-Destructive Children (2nd ed.). Cambridge University Press.
Van Gink, K., van Domburgh, L., Jansen, L., Goddard, N., Ottenbros, R., van der Stegen, B., Popma, A., & Vermeiren, R. (2020). The development and implementation of non-violent resistance in child and adolescent residential settings. Residential Treatment for Children & Youth, 37(3), 176–198.